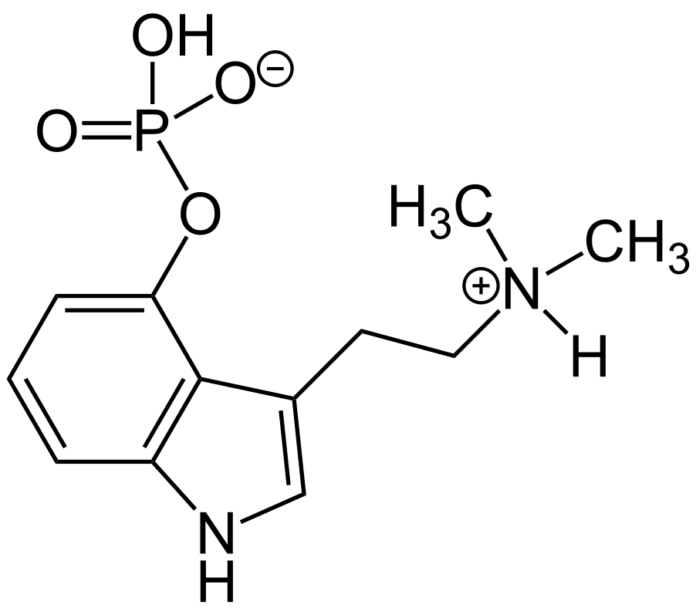
In a groundbreaking move, Australia has become the first country that has allowed psychiatrists to prescribe certain psychedelic substances to patients suffering from depression or PTSD (post-traumatic stress disorder). This significant development marks a turning point in mental health treatment and opens up new possibilities for individuals seeking alternative therapies. With the approval of MDMA (ecstasy) for PTSD and psilocybin (found in psychedelic mushrooms) for hard-to-treat depression, Australia has positioned itself at the forefront of research in this field.
A Paradigm Shift in Mental Health Treatment
The inclusion of MDMA and psilocybin in Australia’s list of approved medicines by the Therapeutic Goods Administration has surprised many scientists. The move signifies a departure from conventional treatment approaches and reflects a growing recognition of the potential benefits of psychedelic substances in addressing persistent mental health issues. Chris Langmead, deputy director of the Neuromedicines Discovery Centre at the Monash Institute of Pharmaceutical Sciences, emphasizes the lack of significant advancements in mental health treatment over the past five decades.
A Global Trend towards Acceptance
Australia’s progressive stance on psychedelic drugs aligns with an international trend toward accepting and exploring their therapeutic potential. Two U.S. states, Oregon and Colorado, have already taken steps to legalize and decriminalize psilocybin, respectively. Moreover, President Joe Biden’s open-mindedness toward psychedelics as a medical treatment has further propelled the discussion on their benefits.
Challenges and Opportunities
While Australia’s decision to allow the prescription of psychedelic drugs is undoubtedly a significant milestone, caution and further research remain essential. American Psychiatric Association has not yet endorsed the use of psychedelics in treatment, highlighting the need for more comprehensive studies and the FDA’s final determination. Medical experts worldwide, including those in Australia, emphasize the importance of understanding the drugs’ efficacy and potential risks, such as hallucinations. Dr. Paul Liknaitzky, head of Monash University’s Clinical Psychedelic Lab, raises concerns about inadequate evidence, clinician competence, treatment affordability, and oversight of training and patient outcomes.